Background
A 350-bed community hospital system in the Midwest reported ending its fiscal year with an $11 million operating income deficit due to the economy and investment losses. Despite reducing operating expenses, a 5% net revenue decline created a negative $5.5 million net income loss for the year. The system CFO stated the hospital had to “do more to control costs and grow revenue to remain financially healthy.” The hospital identified a $16 million need for improvement during the next fiscal year following the loss and targeted between $19 and $34 million in margin improvement the next two years, for a total goal of $35 to $50 million over three years.
Assessment
To better understand the hospital’s challenges; an on-site assessment was done to size, validate, and begin prioritizing margin improvement opportunities. An analysis using data, internal and external benchmarks, and stakeholder interviews confirmed an opportunity for the organization to meet its financial performance improvement goals over the next three years.
Approach
“Immersion” into the hospital’s operations enabled collaboration with hospital leadership to develop specific recommendations, a detailed action plan and timeline with appropriate baseline, and target benchmarks for monitoring progress. Plans were designed with a constant focus on implementation and accountability through coaching and mentoring for sustainable results beyond the engagement. The hospital’s leadership involvement throughout the planning and implementation processes instilled buy-in and created a strong culture of accountability among the management team.
Implementation
Over the course of the project within four months, several critical opportunities for improvement from which action plans were created and implemented included:
- Redesigning several key physician enterprise processes; including revenue cycle, performance-based compensation, elimination of redundant staffing, better referral leakage management, and re-aligned hospital-based physician contract yielded a $13.3 million net income improvement.
- Medical staff education and engagement in Rapid Cycle Improvement using Internal Best Practices resulted in $8.2 million net income improvement.
- Operations improvement; including labor productivity and non-labor (supply chain and facilities management) expense reductions increased net income by $10.5 million.
- Restructuring surgical and oncologic services and implementing new ambulatory programs added $7.1 million in incremental net income.
- Renegotiating key managed care agreements improved net income by $6.1 million.
Results
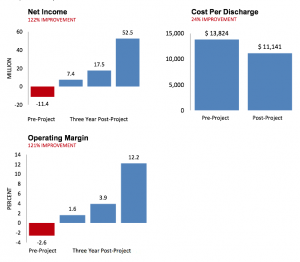
The organization’s significantly improved and sustained operating performance resulted in a $64 million total net income increase in the three years following the engagement. Operating margins improved a total of 14.8% over the post-engagement period – an average increase of nearly 5% per year. Hospital cost per discharge decreased by $2,683 the first year and an average of $1,251 over three years (11%); of which only 11.2% was from labor productivity changes while 75.2% occurred from non-labor expense reduction and process improvements.



